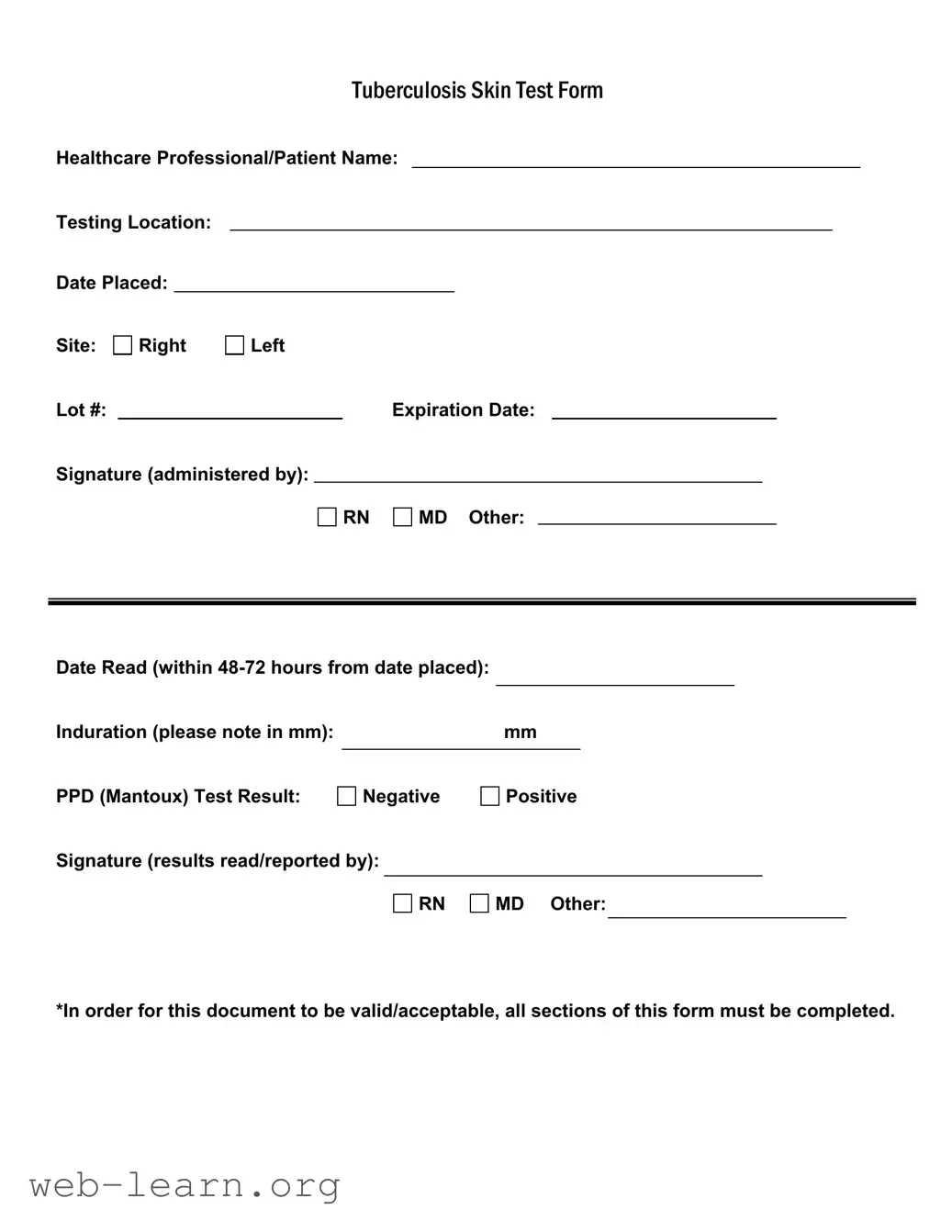
Completing the Tuberculosis (TB) Skin Test form may seem straightforward, yet many individuals encounter common pitfalls that can lead to complications or delays in processing. One frequent mistake occurs during the entry of the testing location. People often forget to specify where the test was administered. This omission can cause difficulties in tracking test results, possibly leading to unnecessary follow-up procedures.
Another common error is the failure to complete the date placed and date read sections accurately. Individuals may accidentally list the wrong date, or they might neglect to write down the date when results were reviewed. Without this information, the validity of the test could be questioned, making it crucial to double-check these entries to ensure compliance with testing protocols.
When it comes to noting the site of the test, confusion can arise. Some may incorrectly mark the right or left side, particularly if they are anxious during the process. This misstep can lead to inaccurate reporting of the test results. Furthermore, improper documentation including the lot number or expiration date of the test can compromise the form’s acceptance. If these details are incorrect or missing, it may necessitate a repeat of the testing.
Completing the induration measurement correctly is critical, as well. Some may misinterpret how to measure this component, either providing an incorrect figure or overlooking the necessity to complete this section altogether. The induration is essential for determining the test result's significance, and inaccuracies here can mislead healthcare professionals.
Signing the form poses another opportunity for error. Individuals might either forget to include the signature of the administering professional or mistakenly choose someone not authorized to sign. Inaccurate signatures can invalidate the form, resulting in additional administrative burdens.
Moreover, many overlook the instructions stating, "In order for this document to be valid/acceptable, all sections of this form must be completed." By assuming that only certain sections need filling out, individuals often submit incomplete forms that are rejected. Adherence to every detail on the form is necessary for it to be processed effectively.
In summary, taking time to carefully review and complete each section of the TB Skin Test form can greatly improve the chances of a smooth testing experience. Attention to detail, particularly in the testing location, dates, site, measurements, and signatures, is required to avoid common mistakes that can disrupt the intended process and lead to unnecessary complications.