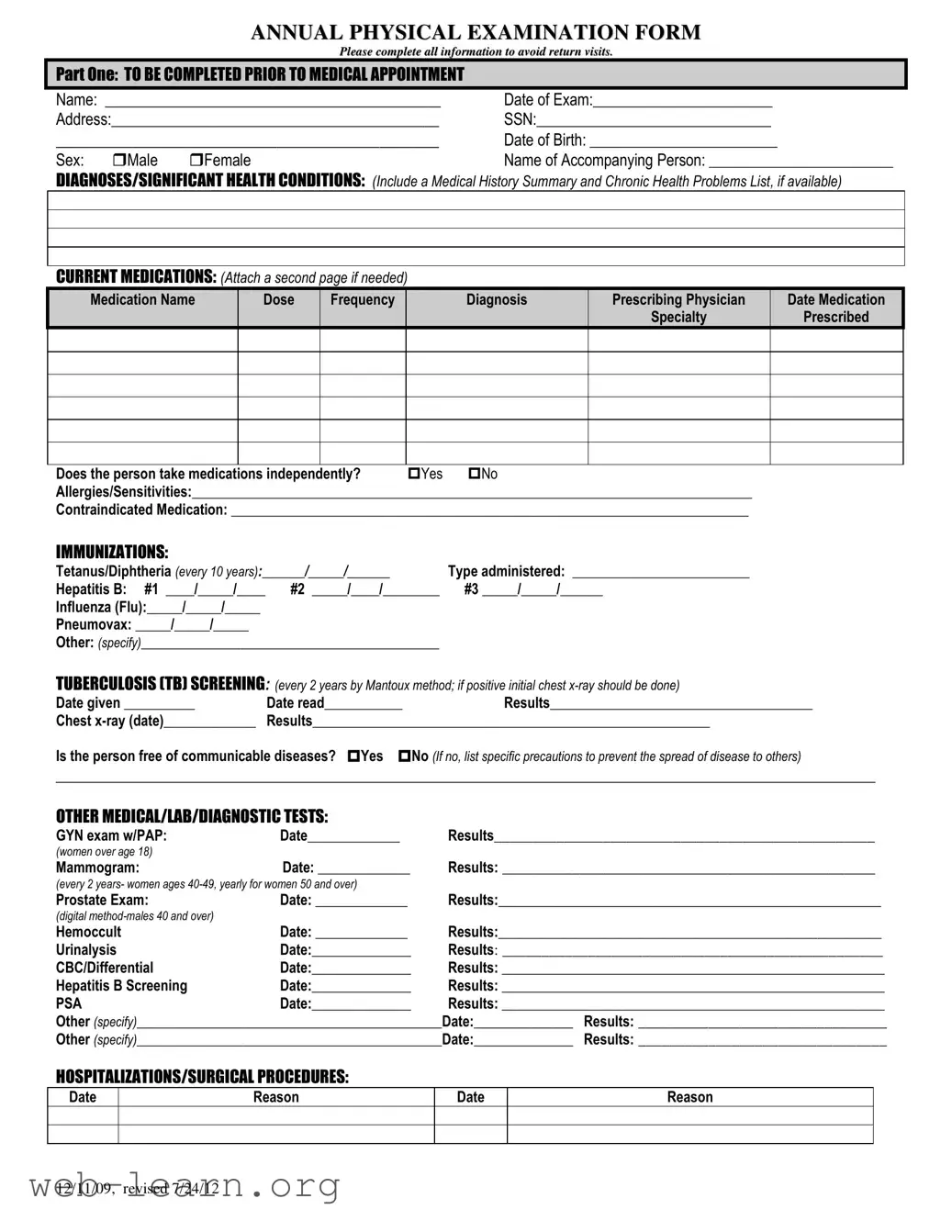
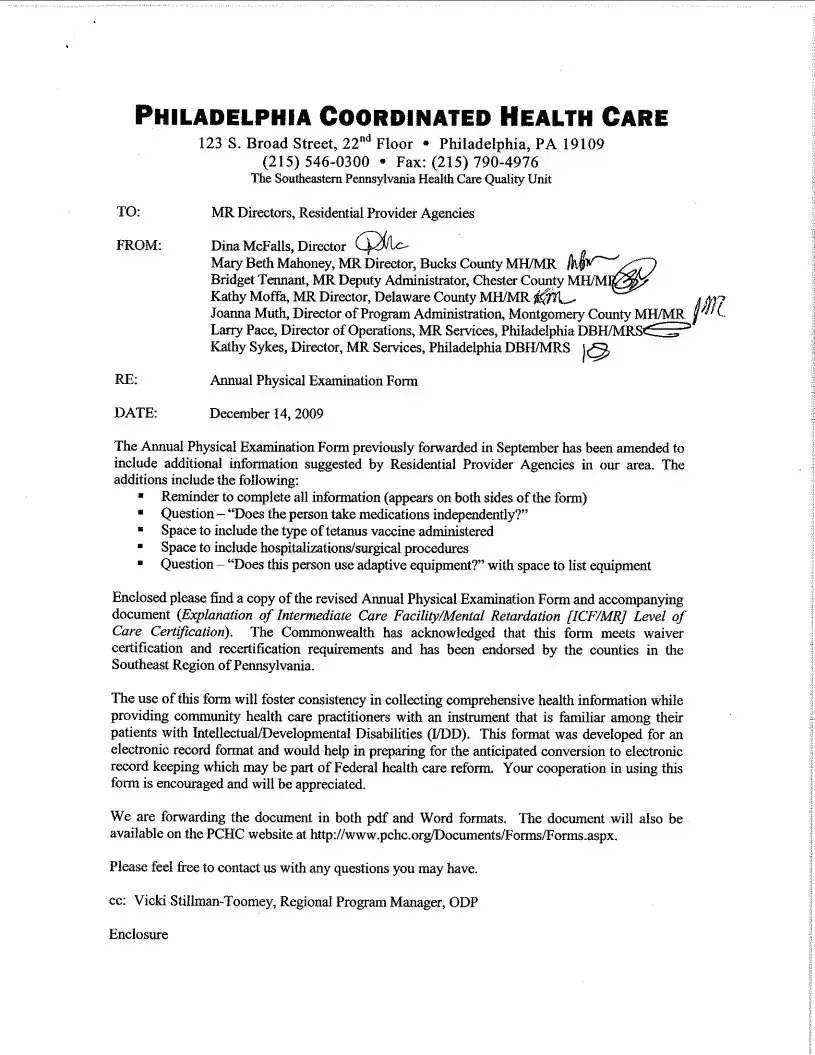
The Annual Physical Examination form serves multiple crucial purposes for both patients and healthcare providers alike. By gathering comprehensive personal information such as the patient's name, date of birth, and contact details, this form establishes a foundational understanding of the individual seeking care. Clinicians can dive deeper into a patient's medical history through sections that request details about diagnoses, significant health conditions, and an overview of current medications. Essential immunization records, including tetanus and flu shots, need to be documented to ensure the patient is adequately protected against preventable diseases. Moreover, it assesses whether any communicable diseases are present, providing an opportunity for proper precautions to mitigate risks. Beyond medical history, the form addresses general physical examination parameters—like blood pressure and heart rate—allowing for an initial snapshot of the individual's health status. Specific tests, including prostate exams for males and mammograms for females, also necessitate documentation to monitor ongoing care. Ultimately, the thorough nature of this form aims to streamline the patient experience and promote effective communication between parties, ensuring that no vital information is overlooked during the examination and subsequent treatments.